Hair removal for Transgender Care
Permanent Choice offers electrolysis and laser hair removal for clients seeking permanent hair removal for cosmetic and surgical purposes.
What is the right option for you?
Electrolysis Vs. Laser Hair Removal
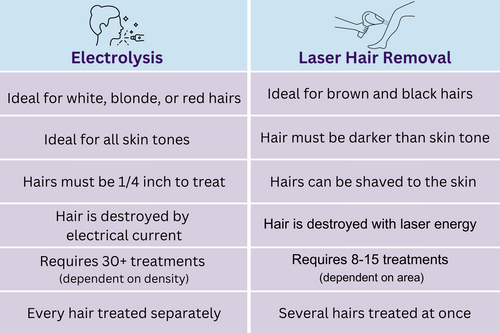
Choosing between electrolysis and laser hair removal depends on various personal factors. Hair color, skin tone, hormones, medications, and hair density all play a role in determining the most effective treatment.
If you are unsure of the best treatment plan for you, we'll assess your specific needs and medical history to create a tailored plan for your hair removal journey during your free consultation.
To meet with a technician and discuss your options, along with what treatment plan would work best for you, book a free consultation today.
Hair removal for the Face and Body
- Our group of specialists are able to provide a custom treatment plan from laser hair removal targeting specific areas to electrolysis for precise results.
- Laser hair removal services, covering facial and body hair, are available in all our locations and by all of our skilled technicians.
- Additionally, electrolysis hair removal for facial hair is also available across all locations, performed by our experienced team.
*Currently we are not taking new electrolysis clients for the body.
Hair removal for Surgical Preparation
Whether Vaginoplasty or Phalloplasty our team of specialists is here to help you prepare for surgery by utilizing laser hair removal and/or electrolysis. Our specialist technicians are well-versed in surgical requirements and client needs, making your hair removal process easy and worry-free.
We recommend allowing at least 12-18 months for hair removal and often advise beginning hair removal around 6 months prior to your first surgery consultation. This allows ample time for hair removal before your surgery date.
Vaginoplasty:
Laser hair removal is recommended to remove hair from the genital area where tissue will be used to create the vaginal canal. The removal process should begin at least a year in advance to ensure enough time for full treatments.
After speaking with your surgeon and determining which technique is right for you, be sure to share that information with your technician. Clients can opt to remove all hair in the pubic and genital areas or just the surgical prep areas.
- *At this time we are only accepting new clients for the method of laser hair removal for vaginoplasty.
- Phalloplasty:
For phalloplasty, hair removal is usually performed on areas such as the forearm or thigh, where skin grafts are taken to construct the phallus. Permanent hair removal treatments are essential to avoid post-surgical complications.
Once you've consulted with your surgeon to determine whether your arm or leg will serve as the donation site, our team can proceed with the appropriate treatment, whether it's laser hair removal or electrolysis.
- *We request that you please bring a diagram of the perimeter required by your surgeon to be removed for surgery, to keep in your file.
- *Please specify if you are preparing for surgery when booking your appointment to ensure you are booked correctly.
Medical Insurance:
Permanent hair removal is increasingly recognized as a medical necessity by insurance companies. Because of this, we encourage clients to contact their insurance companies to inquire if their plans include permanent hair removal for the face, body, or surgical prep areas. It's important to clarify what area(s) and what form of hair removal is covered by your insurance plan and what pre-authorization requirements are needed. Permanent Choice is not able to tell you what is covered under your specific insurance plan, it is the client's responsibility to connect with their insurance providers and get this information.
In-Network Insurance Submission:
Permanent Choice is in-network with Blue Cross Blue Shield of Minnesota (BCBS-MN) as well as HealthPartners (HP), meaning if you are covered by BCBS-MN or HP and your individual plan includes hair removal, we can directly submit claims to your insurance.
Before we can submit your service to your insurance you must contact your insurance provider and confirm that your plan is in-network with Permanent Choice, learn what requirements are associated with your plan to qualify and what areas are covered with your insurance plan.
- * If you have not reached your deductible you will be responsible for the full cost at the time of treatment, which will count toward your annual deductible.
- * You may be responsible for out-of-pocket patient portions of your services.
- * Each insurance plan will require different documentation to qualify you for coverage. Please speak with your insurance company to learn what is required for you to qualify for coverage.
- * We require a copy of the front and back of your insurance card as well as a copy of your PA letter in order to process insurance submissions.
Out-of-Network Medical Reimbursement:
If you do not have BCBS-MN or HealthPartners but your insurance plan includes permanent hair removal you might be eligible for reimbursement.
You will need to contact your insurance provider and inquire if medical reimbursement, also known as in-network benefit exemption, is allowed for your specific plan and what requirements you will need to qualify for this. If you are qualified for medical reimbursement you will be responsible for the full cost of the treatment at each appointment and will receive an insurance invoice which you can use to get reimbursed from your insurance company.
- * Please request your insurance invoice at the end of each treatment. It may take 1-2 business day to receive your receipt via email.
- * If your insurance requires a mailed or faxed invoice please contact our office.
- * It is important to understand how and when to submit a receipt for medical reimbursement and this information can be found through your insurance provider.
- * Medical reimbursement can take 1-3 months to reimburse you for your treatments.
Prior Authorization (PA):
Required by most insurance providers a Prior Authorization, also referred to as precertification, is a determination form made by your healthcare provider regarding the medical necessity of a healthcare service. A PA usually needs to be supported with an MD letter from your doctors or nurses stating the need for gender-affirming hair removal services. This letter can help speed up the process of getting claims approved which is an important aspect of the process. At this time Permanent Choice is not able to submit Prior Authorizations to out-of-network carriers. Please get in touch with your healthcare provider if this is needed.
We advise beginning the approval process for a prior authorization before you start treatments to ensure your treatments are fully covered. In instances where a client's insurance policy covers gender-affirming hair removal, but claims get denied it is often a result of the absence of a PA on record.
Provide the following information to your provider when requesting a PA letter.
- CPT: F64.9
- Laser: 17999
- Electrolysis: 17380
- NPI: 1871165746
- Fax: 9522067599
If you do not find the answers to all of your questions on this page, please call us at (952) 898-1111 and we would be happy to help answer any questions for you.



